Hydrocephalus
A life-threatening brain condition affecting over 1 million Americans
What is Hydrocephalus?
Hydrocephalus (from Greek "hydro" meaning water and "cephalus" meaning head) is a serious brain condition that occurs when cerebrospinal fluid (CSF) builds up to dangerous levels in and around the brain. This fluid buildup typically causes the brain's ventricles to enlarge, creating harmful pressure on brain tissue.
As pressure increases, patients experience severe headaches, sleepiness, paralysis, cognitive problems, and other debilitating symptoms. Without treatment, hydrocephalus leads to coma and death.
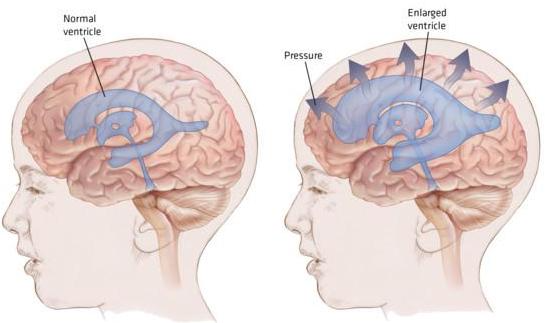
Comparison showing normal brain ventricles (left) versus enlarged ventricles in hydrocephalus (right), demonstrating dangerous pressure buildup.
Affects over 1 million Americans of all ages
Most common reason for brain surgery in children
1 in 770 children born with hydrocephalus annually
800,000 older Americans may have undiagnosed Normal Pressure Hydrocephalus
No cure exists - only surgical management
What Causes Hydrocephalus?
Hydrocephalus develops when there's an imbalance between CSF production and absorption. Most commonly, hydrocephalus is caused by blockages that prevent fluid from flowing normally through the brain's ventricles or into surrounding spaces where it should be absorbed. These blockages can result from blood clots after brain hemorrhages (post-hemorrhagic hydrocephalus), scar tissue from infections, or physical obstructions like tumors or cysts. Less frequently, the brain loses its ability to absorb CSF effectively, often due to inflammation from infection or injury. Rarely, the brain produces too much fluid. Some people are born with developmental abnormalities that disrupt normal fluid flow, while others acquire the condition later due to trauma, tumors, infections, or stroke.
Congenital Hydrocephalus
Present at birth due to developmental problems during pregnancy:
- Spina bifida - Most common cause; affects brain and spine development
- Aqueductal stenosis - Narrowing of the pathway between brain ventricles
- Brain malformations - Dandy-Walker syndrome, Chiari malformation
- Prenatal infections - Rubella, toxoplasmosis, or other maternal infections
Acquired Hydrocephalus
Develops after birth due to injury or disease:
- Post-hemorrhagic hydrocephalus - Blood clots from brain bleeding block fluid pathways
- Head trauma - Car accidents, falls, sports injuries, or violence
- Brain tumors - Masses that block cerebrospinal fluid pathways
- Stroke - Disrupts normal brain fluid circulation
- Central nervous system infections - Meningitis, encephalitis
- Idiopathic - No identifiable cause, especially in older adults
The Hidden Epidemic: Normal Pressure Hydrocephalus
A staggering 800,000 older Americans may be living with undiagnosed Normal Pressure Hydrocephalus (NPH), with more than 80% of cases remaining unrecognized or untreated. Many are misdiagnosed with Alzheimer's disease when they actually have a treatable condition.
Real-Life Impact
Kate Finlayson - Our Inspiration
Kate, who inspired Team Hydro's formation, developed hydrocephalus as a premature baby. Despite enduring over 100 surgeries, multiple strokes, and countless hospitalizations, she lived courageously until age 26. Her story exemplifies both the challenges and resilience of those living with hydrocephalus.
Congresswoman Gabby Giffords
Developed hydrocephalus following gunshot wounds to the head, demonstrating how traumatic brain injury can lead to this condition.
Billy Joel
The legendary musician was diagnosed with Normal Pressure Hydrocephalus (NPH) in 2025. His openness about the diagnosis helps raise awareness for NPH, which affects hundreds of thousands of older Americans but often goes unrecognized or is misdiagnosed as Alzheimer's or Parkinson's disease.
Current Treatment Limitations
The primary treatment is surgical insertion of a shunt - a device that drains excess fluid from the brain to other parts of the body. While life-saving, shunts present significant challenges.
A shunt system consists of a catheter placed in the brain's ventricles, connected to a valve that regulates flow, and tubing that carries the excess fluid to another part of the body (usually the abdomen) where it can be safely absorbed.
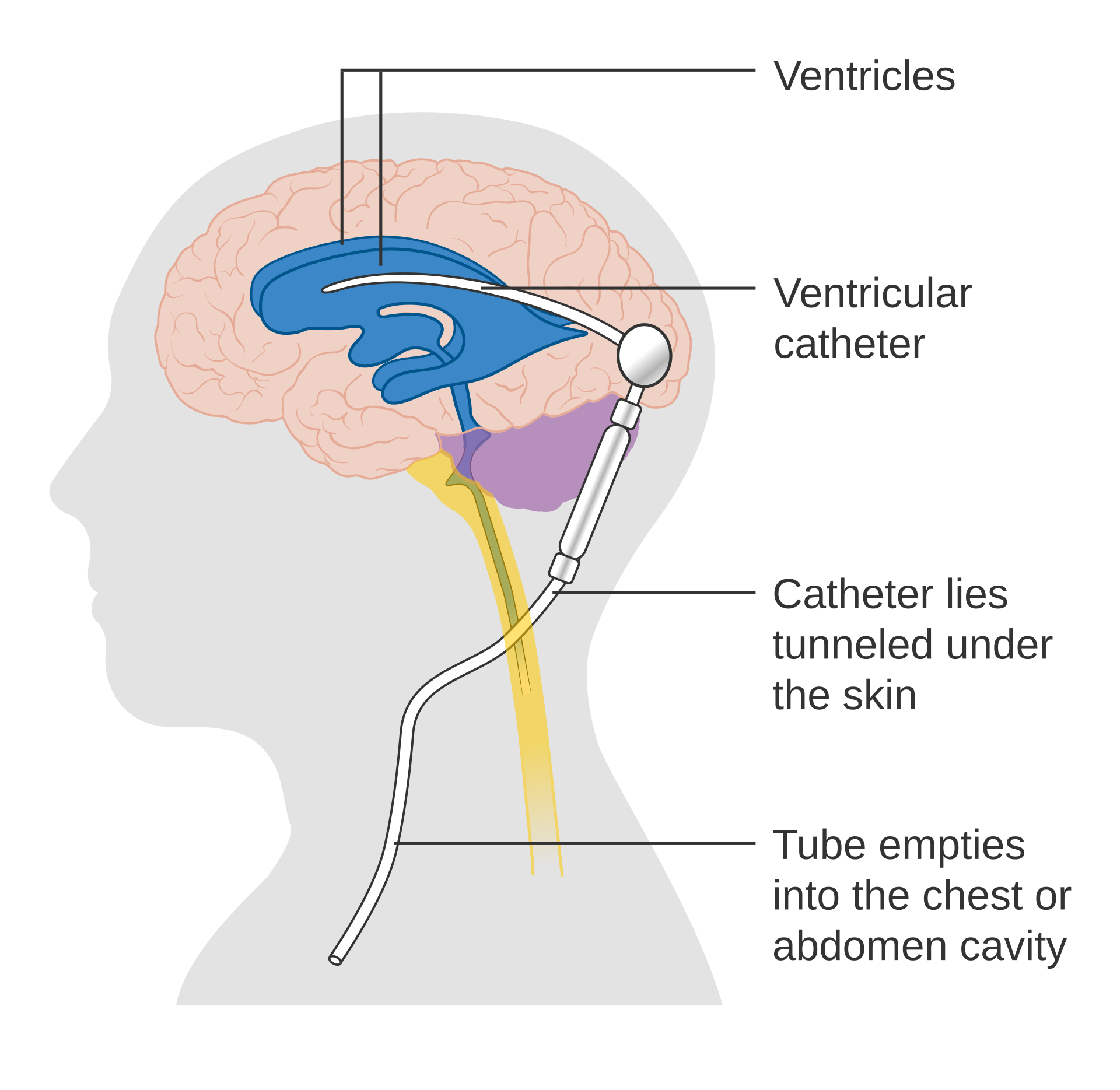
A shunt system drains excess fluid from the brain's ventricles through tubing that runs under the skin to the abdomen or chest cavity.
The statistics are sobering: 50% of all shunts fail within two years, requiring emergency brain surgery to replace or repair them. The United States performs approximately 40,000 shunt-related operations annually - that's one surgery every 13 minutes, or over 100 procedures daily. These operations cost over $1 billion per year, yet the National Institutes of Health allocates only $1 million annually to hydrocephalus research.
The Harsh Reality of Shunt Complications
Blockage
Can cause rapid brain damage and requires emergency surgery. Signs include severe headaches, vomiting, and altered consciousness.
Infection
More common in the first months after surgery. Can cause fever, redness along the shunt, neck stiffness, and requires antibiotics or shunt replacement.
Mechanical Failure
Shunt components can break, disconnect, or migrate. Children may outgrow their shunts as they develop.
Over/Under-drainage
Too much or too little drainage can cause seizures, bleeding, or cognitive problems.
Alternative surgical options include Endoscopic Third Ventriculostomy (ETV), where surgeons create a small hole in the brain's ventricle floor to allow natural drainage, and ETV with Choroid Plexus Cauterization (CPC), which also reduces fluid production. However, these procedures have similar failure rates to shunts, with holes closing unexpectedly and requiring emergency conversion to shunt systems.
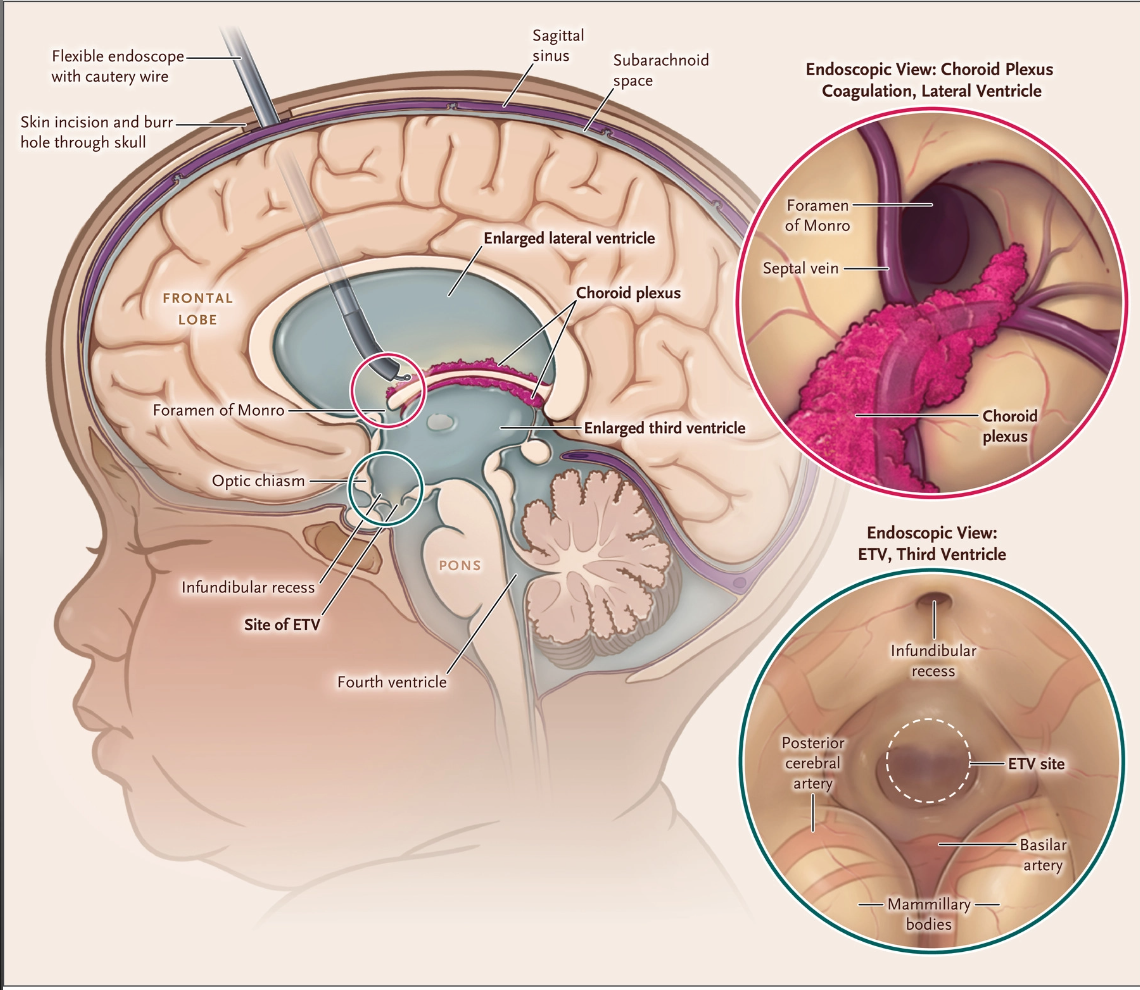
ETV creates a drainage hole in the brain's ventricle floor, while CPC reduces fluid production by cauterizing the choroid plexus.
Researchers have investigated various medications to treat hydrocephalus non-surgically, including drugs to reduce fluid production or improve absorption. However, no effective pharmaceutical approach has yet been established, leaving brain surgery as the only effective treatment option for hydrocephalus patients today.
Imagine undergoing brain surgery every few years just to survive. This is the reality for people with hydrocephalus.
The Daily Reality of Living with Hydrocephalus
People with hydrocephalus are vibrant individuals pursuing meaningful lives while managing constant uncertainty. They live knowing their shunt could fail at any moment, requiring immediate emergency surgery.
Infants and Children
- Rapid head growth and developmental delays
- Learning disabilities and school performance challenges
- Seizures and coordination problems
- Multiple surgeries disrupting childhood
Adults
- Chronic headaches affecting work and relationships
- Memory problems and difficulty concentrating
- Balance issues and vision problems
- Career limitations due to unpredictable medical needs
Older Adults with NPH
- Progressive cognitive decline mistaken for dementia
- Loss of independence due to walking difficulties
- Social isolation from embarrassing bladder problems
- Delayed diagnosis leading to irreversible damage
Living in Emergency Mode
Families must be constantly vigilant for signs of shunt failure: sudden severe headaches, vomiting, confusion, or changes in behavior. These symptoms can progress rapidly from discomfort to life-threatening emergency within hours. Parents become expert medical observers, children miss school for numerous hospital visits, and adults carry medical alert cards everywhere they go.
The Urgent Need for Research
Despite affecting over a million Americans and costing healthcare systems billions annually, hydrocephalus remains severely under-researched. Current treatments, largely unchanged since the 1950s, represent outdated solutions to complex neurological problems.
70 Years of Technological Stagnation
Consider this: The basic shunt technology we rely on today was developed in the 1950s. While we've put computers in our pockets and sent robots to Mars, people with hydrocephalus still depend on crude drainage tubes that fail regularly and require dangerous brain surgery to fix.
Join the Fight to End Hydrocephalus Suffering
Imagine a world where hydrocephalus could be treated with a pill instead of brain surgery. Where children wouldn't face a lifetime of medical uncertainty. Where families wouldn't live in fear of the next shunt failure. This is what research can achieve.
The research gap is shocking, but together we can change this. Every dollar donated to Team Hydro goes 100% directly to hydrocephalus research - funding the breakthrough discoveries that could transform or save lives.